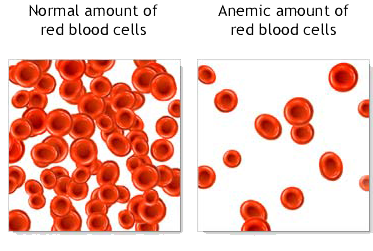
- Hemoglobin 10.5 (WHO normal 14.0-17.3)
- Absolute neutrophil count 0.8 (normal 1.4-7.5)
- White blood cell count 1.7 (normal 4-10)
- Red blood cell count 3.06 (normal 4.5-5.9)
- Platelet count 103 (normal 150-450)
Lots of irritating stumbling blocks. Dr. B canceled an appointment, but nobody told me until I arrived at the hospital. Explanation (or excuse): we thought you were being treated elsewhere. Not true — I was still deciding, and the decision hung on whether my doc here would continue to treat me like his own patient. Felt very much like a door being slammed in my face.
More unreturned phone calls. Finally on Tuesday I went in for another blood test. I'm Dr. B's new nurse, said the very nice person who brought out the lab results. I understand you're being treated elsewhere. So I went through the whole story again, for the 10th time: no, not yet. Want to do it, but first, need to know that the arrangements for drugs and infusions will work. The docs have to talk. Above all, I don't want to do it if Dr. B won't keep treating me here.
The other nurse was OK, but this one seemed to genuinely listen. She made a lot of notes and went off immediately to contact with Dr. B. 3 hours later, the docs had talked. The path starts to look smoother.
Now, lots and lots of logistics. Flying to DC, staying there Nov. 8-14, getting all the cladribine infusions down there since our infusion center isn't open on Sundays.
 My partner's coming down on Tuesday night, staying the rest of the week so she can be there for the treatments. Meanwhile my amazing-but-true mother's coming up here to take care of Luka the ninja warrior, who turns 8 next week. On Friday, she and Luka will fly to DC as well; Luka can see the White House and the Air & Space Museum, and, oh yeah, his dad.
My partner's coming down on Tuesday night, staying the rest of the week so she can be there for the treatments. Meanwhile my amazing-but-true mother's coming up here to take care of Luka the ninja warrior, who turns 8 next week. On Friday, she and Luka will fly to DC as well; Luka can see the White House and the Air & Space Museum, and, oh yeah, his dad.Some good days, some bad days. Yesterday I made it through most of a 7-hour faculty retreat, but couldn't quite manage the last hour. Went home and took a nap. Headaches hanging around, stormclouds on the horizon; not always active, but always possible.